Product Research
Product research drives what we do. Our product research initiatives encompass:
- Domain and Market Assessments to determine what is required, what daunting problems are to be solved and what technology to be used in building out a successful product.
- Opportunity Assessment to help understand demand, model the go to market strategy and evaluate how much of a value addition can the product bring to a business or enterprise.
Our research processes and deliverables are crafted to evaluate new ideas, product development strategies, key concepts and decisions to ensure there is no costly rework.


Product Conceptualization
A plan for realization of products and solutions is always driven by conceptual studies. At Novacis, all ideas and concepts are critically evaluated for their relevance, sustainability and aligned with the results of product research. Product Conceptualization focusses on:
- Validate Product Research
- Create Proof of Concepts (POCs) and Proof of Value (POVs)
- Technology and Engineering Considerations
- Prototyping
- Artefact creation
- Domain and Technology Pilots
Product Engineering
We truly engineer products! At Novacis, we take care of the entire product life cycle from the innovation phase, starting from the idea being conceived to the deployment and business improvement tracking. Emphasis of product engineering aspects will be in the following phases:
- Functional Engineering
- Usability Engineering
- Architecture and Design
- Solution Pilots and Prototypes
- Release Management
- Product Packaging
- Product Quality Assurance
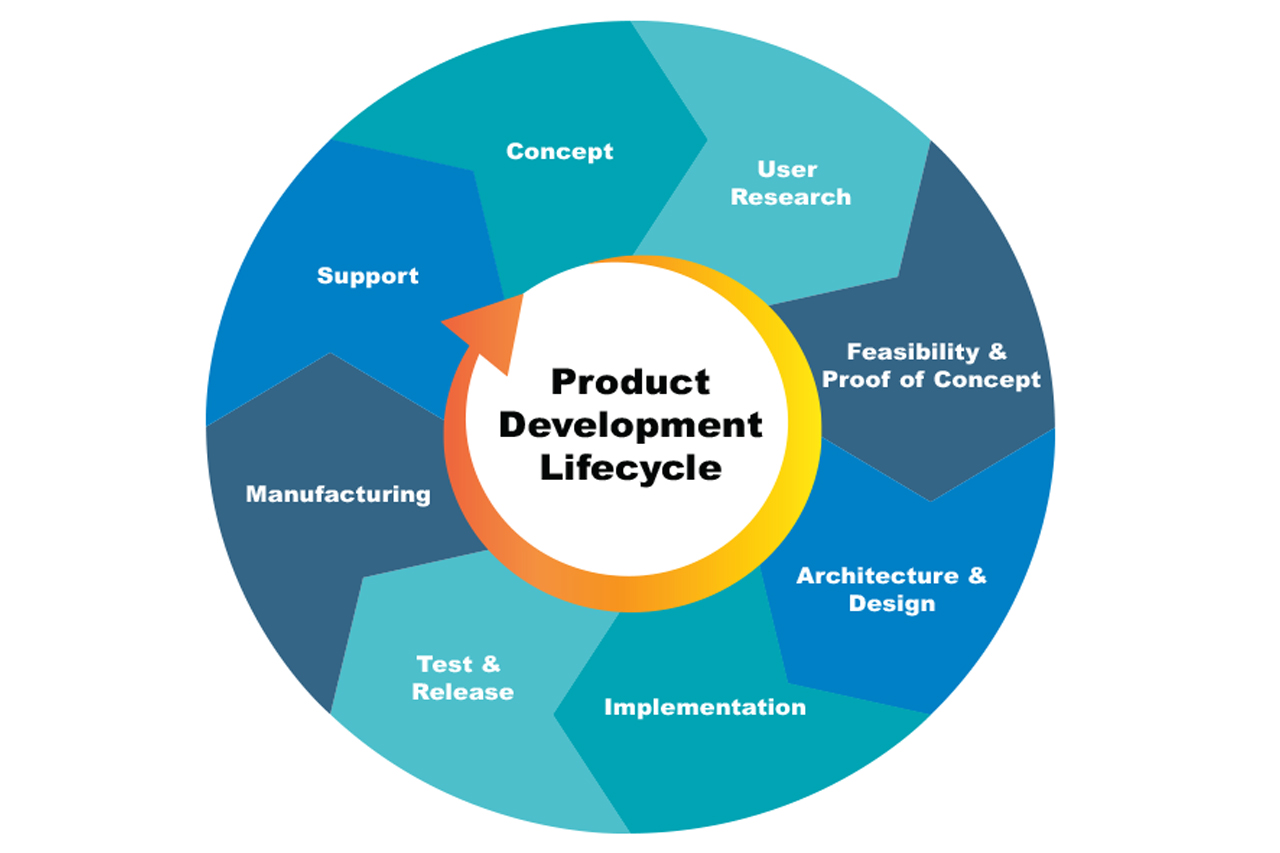
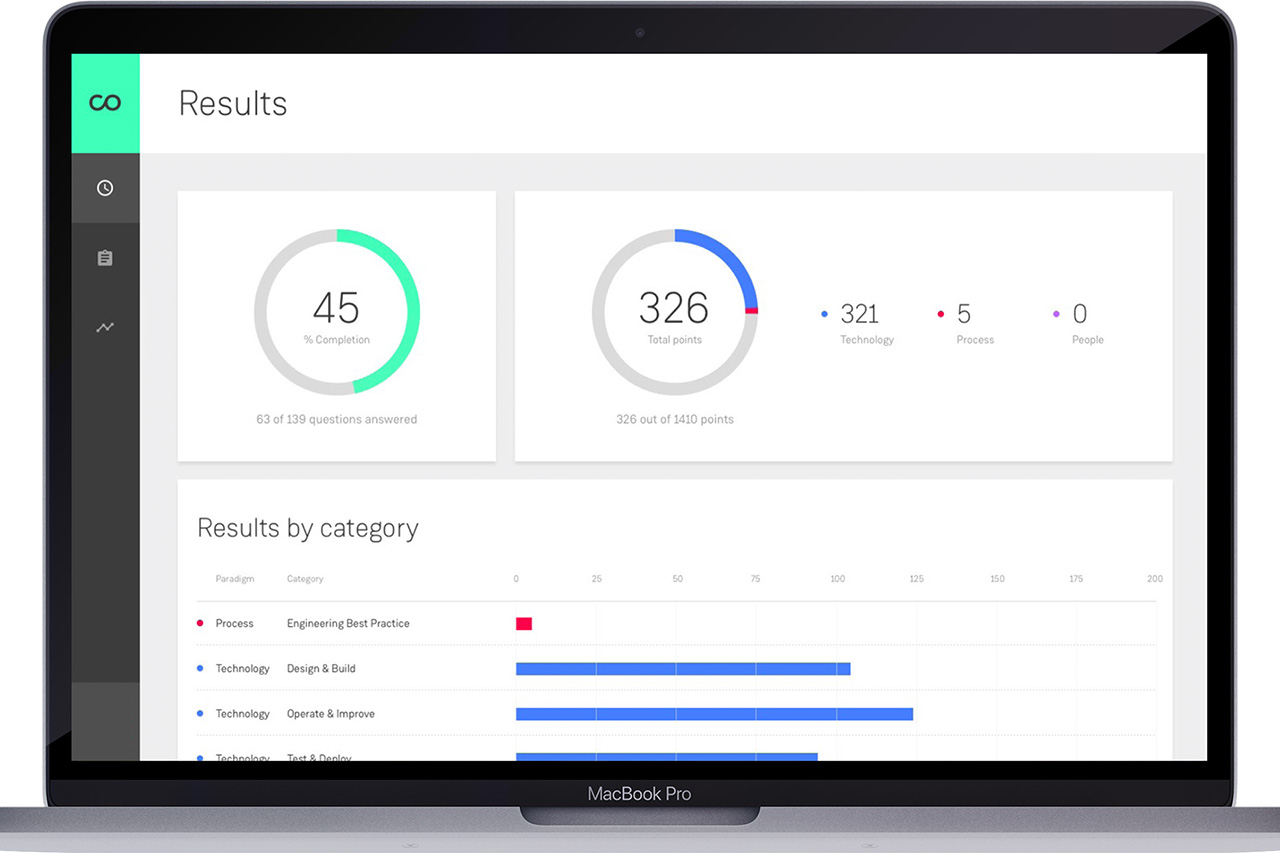
Product Development
Product development processes at Novacis focusses on all of the following aspects:
- Product roadmap and product management planning
- Product scoping and functional engineering
- Product design and development
- Product release management
- Product support
Our product development process is modelled and finetuned by standard product engineering practices that advocate for planning, structured execution and successful delivery in adherence to a futuristic product roadmap.
Product Packaging
Novacis’ product packaging processes and documentation focus on producing quality product packaging deliverables. A successful deployment of our solution is followed by the delivery of one or more of the following:
- Product Documentation
- Product Collaterals
- Training Kits